Resources
FAQ: Helping your Registrar manage Patients with Long COVID
This webpage complements the webinar recordings on this topic, available either via our YouTube channel or in audio format by clicking on the corresponding button below:
Let’s start with a case study

Identifying Long COVID
During your weekly teaching session, Nicole, your GPT1 registrar, asks you about a patient she has seen with ‘possible long COVID’:
- 46-year-old woman
- works as a hospital cleaner
- PCR confirmation of COVID infection 8 weeks earlier
- acute respiratory illness lasted 5 days
- since respiratory illness settled, has experienced:
- persistent fatigue
- ‘brain fog’
- muscle aches
- has missed a number of days of work over this period
Nicole says that “it sounds like Long COVID”, but admits she has never managed anyone with this before. She asks for your advice on how to proceed.
Apart from clinical care, what broad themes of quality general practice should be considered when responding to a registrar in Nicole’s situation?
What does the registrar need to learn?
Learners will come with learning needs – mainly those they want to learn. These are driven by identified knowledge and skill gaps, and exams…
But there are many things they need to learn.
The RACGP uses the star analogy to describe general practice through 5 domains of general practice: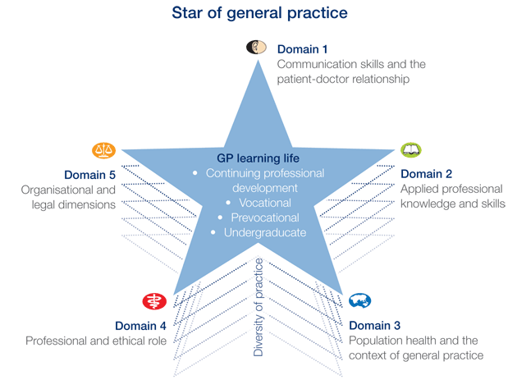
How would you help Nicole address the Unknown Unknowns in this scenario?
Teaching the registrar about uncertainty in the context of Long COVID
- Accept that uncertainty is inevitable
- Gather sufficient data
- Identify the patient’s agenda
- Reason analytically
- Share decision-making
- Seek evidence
- Safety net


Why is Nicole asking for help?
What is the registrar really asking of you?
"Save me!"
"Help me!"
"Reassure me!"

How can the PQRST framework be used here?
What is the PQRST model?
P – What is the patient’s problem?
Q – What is the registrar’s question?
R – How well does the doctor reason?
S – What is the solution?
T – What can be taught?
Resources for Clinicians
* Australian Government Department of Health and Aged Care: Medical Research Future Fund Report on the Coronavirus Research Response (May 2023)
* National COVID-19 Health and Research Advisory Committee: Advice 29 - Update on Long COVID

What resources would you first point Nicole to?
Existing resources
RACGP clinical resources
Guidelines: caring for patients with post-COVID-19 conditions
Patient resource: managing post-COVID-19 symptoms
National Clinical Evidence Taskforce (NCET)
NCET guidelines
NCET flowchart on care of people after COVID-19
Jurisdictional Health Department resources
ACT -
NSW -
Vic -
QLD -
Tas -
SA -
WA -
NT
Resources for Consumers
* Healthdirect: Understanding post-COVID-19 symptoms and long COVID
* World Health Organization (WHO): Support for rehabilitation: self-management after COVID-19-related illness
* Emerge Australia: Long COVID
* Beyond Blue: COVID-19
Frequently Asked Questions
The term ‘long COVID’ is generally used to describe both:
- Ongoing symptomatic COVID-19 – COVID-19 symptoms lasting more than 4 weeks
- Post-Acute Sequelae of COVID-19 (PASC), also known as post-COVID-19 condition/syndrome
“Post COVID-19 condition occurs in individuals with a history of probable or confirmed SARS-CoV-2 infection, usually 3 months from the onset of COVID-19 with symptoms that last for at least 2 months and cannot be explained by an alternative diagnosis.
Common symptoms include fatigue, shortness of breath and cognitive dysfunction, as well as others that generally have an impact on everyday functioning. Symptoms may be new onset, following initial recovery from an acute COVID-19 episode, or persist from the initial illness.”
- PASC is an emerging health issue, both in Australia and internationally.
- Uncertainty remains regarding the prevalence of PASC in Australia.
- Due to Australia’s unique context, the prevalence and impact of PASC will likely differ from that experienced internationally.
- PASC develops in patients after the acute phase of COVID-19, regardless of initial disease severity.
- It is a multisystemic condition with unclear pathogenesis.
- With more than 200 symptoms described in the literature, patient presentation varies.
Symptoms can be episodic and may fluctuate or relapse over time. - Known risk factors include:
- Female sex
- Older age
- Not being up-to-date with vaccination against COVID-19
- Severity of initial COVID-19 infection
- Pre-existing co-morbidities
- A current challenge with diagnosing PASC is the lack of consensus regarding classifications and diagnostic criteria.
- No PASC specific diagnostic tests are currently approved in Australia.
- If a diagnostic test was developed, it would require evaluation under the Therapeutic Goods Administration’s in vitro diagnostic regulatory framework.
- To be funded under Medicare, the Medical Services Advisory Committee would need to assess its comparative safety, clinical effectiveness, cost-effectiveness, and total cost, and provide advice to Government.
- There are no medicines currently listed on the Pharmaceutical Benefits Scheme for the treatment of PASC.
- Medicines may be available to treat symptoms related to PASC.
‘Sick and Tired: Casting a long shadow’ summary of report recommendations:
- Improving data and data linkage on COVID-19 including long COVID through a single COVID-19 database
- A definition of long COVID for interim use in Australia
- Evidence-based guidelines for diagnosis and treatment co-designed with patients with lived experience
- A nationally coordinated research program for long COVID and COVID-19
- Improving COVID-19 vaccination communications for all population groups
- Continuing to review the benefits of, and expanding access to, antiviral treatments for COVID-19
- Improving the support provided to people experiencing long COVID with a focus on primary care supports
- Indoor air quality and ventilation
- The central role of primary care, particularly GPs, in management of people with PASC was emphasised throughout the Inquiry given:
- A large proportion of patients with PASC have chronic symptoms.
- PASC is considered to be a multisystem disease that can have psychosocial impacts.
- Most people with PASC can be effectively managed through primary care services.
- A small number of patients may require other (non-GP) specialist care.
- People with PASC symptoms are likely to seek review from their GP in the first instance.
- GPs have a key role in diagnosing, managing and supporting people with PASC.
- For those requiring multidisciplinary care, GPs play an important role in referring patients to allied health services and coordinating ongoing patient management.
- To be effective, primary care needs to be supported with education, specialist input, guidelines and resources.
- Most people with PASC will receive management and support through primary care.
- The Department of Health and Aged Care is developing a National PASC Plan. The Plan will be informed by:
- Input from a number of areas across the Department
- Recommendations handed down by the Committee
- Key aims of the Plan are to:
- Improve health system ability to deliver models of clinical care to people living with PASC
- Develop PASC health resources for the public and healthcare providers
- Support research to increase our knowledge of PASC and guide future policy and clinical care
- The plan will be part of the Australian Government’s formal response to the Committee’s findings.
Date reviewed: 15 April 2025
Please note that while reasonable care is taken to provide accurate information at the time of creation, we frequently update content and links as needed. If you identify any inconsistencies or broken links, please let us know by email.